Immediate medical attention is important if you have a subdural hematoma. So, what is a subdural hematoma, and how can you tell if you have one? A subdural hematoma is a serious type of brain injury that occurs when blood accumulates between the brain and its outer protective covering. You may have few or no symptoms at first, though common symptoms include headaches and slurred speech.
If you or a loved one has suffered a subdural hematoma due to someone else’s negligence, an accident, or medical malpractice, you may be entitled to significant compensation. Easton, PA catastrophic injury attorney Shaughnessy has successfully handled numerous brain injury cases and understands the complex medical and legal issues involved. Time is critical in these cases, so don’t wait to contact The Law Offices of Edward P. Shaughnessy. Call today at (610) 258-9955 or contact us online to schedule your free consultation.
Understanding Subdural Hematomas
A subdural hematoma occurs when blood seeps into the subdural space between the dura mater and arachnoid mater. Bleeding can result from sudden acceleration or deceleration forces, causing the brain to move within the skull and tearing the bridging veins that connect the surface of the brain to the dura mater. The accumulated blood increases intracranial pressure, potentially leading to brain damage, coma, or death if left untreated.
Subdural hematoma differs from other types of brain bleeds primarily in their location and the blood vessels involved. For example, intracerebral hemorrhages occur within the brain tissue itself rather than in the space between the brain and its protective layers. Subarachnoid brain hemorrhages, which occur in the subarachnoid space, typically involve arterial bleeding rather than bleeding caused by blood vessels breaking. The venous nature of most subdural hematomas often means they sometimes develop more slowly than arterial bleeds. However, they can still cause severe neurological complications due to the gradual increase in pressure on the brain.
Epidural vs Subdural Hematoma
The key differences between epidural and subdural hematomas lie in their anatomical location and the typical circumstances that cause them. An epidural hematoma occurs between the bony skull and the dura mater (the brain’s tough outer lining). A subdural hematoma develops under the skull, between the dura mater and the arachnoid membrane. Epidural hematomas are often associated with skull fractures and arterial bleeding, particularly from the middle meningeal artery. This can cause rapid deterioration and require immediate surgical intervention. Subdural hematomas happen from venous bleeding caused by the tearing of the bridging veins that span the subdural space. These can occur with or without skull fractures.
Types of Subdural Hematomas

Subdural hematomas are classified into three distinct types based on how fast the condition develops as well as how much bleeding and damage occur. The classification system helps medical professionals determine the urgency of rapid treatment and predict potential outcomes for patients.
Acute Subdural Hematoma
Acute subdural hematomas, the most dangerous type, develop within minutes to hours following a head injury. These injuries typically result from high-impact trauma such as car crashes, severe falls, or violent assaults. The quick buildup of blood creates immediate pressure on the brain, leading to rapid neurological deterioration that can be life-threatening within hours. Emergency surgical intervention is typically required to relieve pressure on the brain.
Chronic Subdural Hematoma
Chronic subdural hematomas develop slowly over weeks to months. Elderly patients, individuals with brain atrophy, and those taking blood thinners are particularly vulnerable to this condition even after mild head injuries. The slow bleeding allows the brain to gradually adapt to the increasing pressure, which is why symptoms may not manifest right away. Delayed presentation makes chronic subdural hematomas particularly challenging to diagnose. This condition may be mistaken for other conditions, such as dementia or normal aging.
Subacute Subdural Hematoma
Subacute subdural hematomas have characteristics that fall between acute and chronic presentations. Individuals usually experience symptoms within days to weeks after initial injury. The development of subacute subdural hematomas can be unpredictable, with symptoms sometimes initially improving before worsening as the hematoma expands. This fluctuating pattern can make diagnosis particularly challenging for healthcare providers and may lead to delays in appropriate treatment.
What Causes Subdural Hematomas?
Head trauma is the primary cause of subdural hematomas. This condition can result from a latent brain injury after a car accident or a slip-and-fall accident. Workplace accidents involving falling objects, safety equipment malfunctions, or falls from elevated surfaces can also result in injuries that lead to hematomas. Contact sports like football, hockey, or boxing often cause repeated head impacts that may lead to subdural bleeding. Medical malpractice cases may involve subdural hematomas caused by surgical errors or improper medication management. Physical assaults, child abuse, and domestic violence incidents frequently result in subdural hematomas when victims suffer blunt force trauma to the head. Infants specifically may experience subdural hematomas related to shaken baby syndrome.
Subdural Hematoma Risk Factors
Certain factors increase an individual’s likelihood of developing a subdural hematoma, even from minor head injury. Being aware of risk factors is key to preventing subdural hematomas. Age is a major risk factor, with older adults and young children at the highest risk level. In elderly patients, natural brain shrinking creates more space between the brain and skull, making bridging veins more susceptible to tearing. Infants and children have larger heads and weaker neck muscles, making them vulnerable to brain injuries from impact or shaking. The elderly also have more fragile blood vessels and slower healing, increasing complications from subdural bleeding.
Those with previous brain injuries have a higher risk due to weakened blood vessels and scar tissue that makes the brain more susceptible to bleeding. Repeated head trauma from contact sports or abuse causes cumulative damage that increases the likelihood of bleeding.
Medical conditions affecting blood clotting or brain structure can significantly increase subdural hematoma risk. Bleeding disorders like hemophilia or liver disease impair clot formation, making minor head trauma dangerous. Conditions affecting blood vessel strength, such as hypertension, make blood vessel rupture more likely. Untreated cerebrospinal fluid leaks can also lead to subdural hematomas. Additionally, blood-thinning medicines prevent blood clots but can cause repeated bleeding when injuries occur, potentially turning minor head trauma into life-threatening hematomas.
Symptoms of a Subdural Hematoma

Common symptoms of a subdural hematoma include headaches, confusion, and dizziness. Some individuals experience nausea, vomiting, and loss of consciousness. Slurred speech, difficulty balancing or walking, and vision problems may also occur. Extreme cases may involve seizures. Chronic subdural hematomas in particular can result in persistent symptoms such as memory loss, disorientation, and personality changes.
You should always go to the doctor after an accident, even when you feel fine. A medical professional will know how to diagnose and treat subdural hematomas as well as the underlying brain injury.
How Is a Subdural Hematoma Diagnosed?
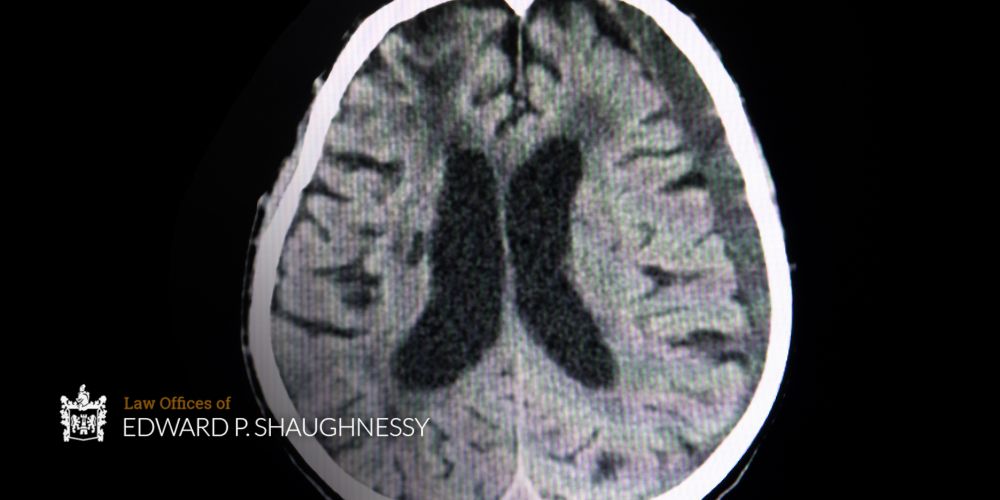
Subdural hematomas can present like stroke, brain tumors, dementia, or psychiatric conditions. The gradual onset of symptoms in chronic cases can be mistaken for normal aging or depression, particularly in elderly patients. Prompt identification can mean the difference between full recovery and permanent disability or death. CT scans quickly reveal blood in the subdural space and brain compression. MRI provides more detailed images, particularly useful for smaller or chronic hematomas.
How Is a Subdural Hematoma Treated?
Treatment depends on the type and severity of the subdural hematoma. Severe cases causing significant brain compression require immediate surgical intervention. Craniotomy involves removing skull bone to access and remove the hematoma. Burr hole drainage uses tubes inserted through small skull holes to drain blood, often used for chronic hematomas. Smaller hematomas may be managed with close neurological monitoring, blood tests to measure clotting function, and physical exams in hospital settings. Medications may include anti-seizure drugs, pain medications, and drugs to reduce brain swelling and control symptoms.
Many patients require extensive rehabilitation for full recovery. This can include physical therapy for strength and mobility, occupational therapy for daily living skills, speech therapy for communication, and cognitive rehabilitation for memory and problem-solving skills. Immediate care is key to recovering from a hematoma. Delayed treatment allows continued bleeding and brain herniation, leading to irreversible damage.
Long-Term Effects of a Traumatic Brain Injury
Potential long-term effects of TBIs include a wide range of physical, mental, and emotional issues. Individuals may experience motor function problems like weakness, paralysis, poor coordination, and balance difficulties. Vision or hearing problems, chronic headaches, and fatigue are also common. Some experience issues with cognitive brain functions such as memory, attention, and concentration. Additionally, brain injuries may lead to mental disorders later in life. This can lead to personality changes, emotional regulation problems, depression, anxiety, and irritability. Many survivors face permanent limitations in work ability, relationships, or independent living. The combination of physical, cognitive, and emotional deficits can require lifelong care assistance, adaptive equipment, or specialized housing arrangements.
Types of Damages for Subdural Hematoma Injuries in Pennsylvania
Victims who suffer subdural hematomas caused by another person’s negligence or intentional acts can recover various economic and non-economic damages. Economic damages cover financial losses with specific dollar amounts. This includes compensation for medical expenses, wages lost during recovery, and loss of earning capacity when permanent disabilities prevent you from earning the same income as before. Non-economic damages compensate for losses that don’t have a specific price tag but significantly impact your quality of life. This includes compensation for pain and suffering, mental anguish, and emotional distress caused by the head injury. Loss of consortium damages may be available to family members who have suffered the loss of companionship or support due to the injured person’s condition.
Why You Need an Easton, PA Traumatic Brain Injury Lawyer
TBI cases require an understanding of complex medical concepts and long-term implications that general personal injury attorneys may lack. An Easton traumatic brain injury lawyer has relationships with medical experts, neuropsychologists, and life care planners who provide crucial testimony. Their specific experience in representing victims of TBIs gives their clients an advantage, helping them pursue maximum compensation.
Skilled attorneys know how to obtain and interpret complex medical records and imaging studies. They understand insurance company tactics to minimize payouts and can effectively counter lowball offers with solid evidence and expert testimony. TBI lawyers help families navigate the healthcare system, connect with medical specialists, and ensure settlement agreements include provisions for future needs.
Subdural Hematoma FAQs
Is a Subdural Hematoma The Same As A Subdural Hemorrhage?
Although the terms are used interchangeably, a hemmorage typically refers to active bleeding while a hematoma is a collection of blood.
How Common Are Subdural Hematomas?
Subdural hematomas occur in approximately 25% of people with head injuries.
Is Subdural Hematoma a Stroke?
No. A subdural hematoma is bleeding outside the brain that presses on brain tissue, while a stroke involves interrupted blood flow in the brain.
Suffered a Subdural Hematoma? Call Easton, PA Traumatic Brain Injury Lawyer Ed Shaughnessy Today

Brain injuries can have devastating, life-altering consequences that extend far beyond the initial medical emergency. The mounting medical bills, lost income, and need for long-term care can quickly overwhelm families already dealing with the trauma of a severe head injury. Seek the help you need from The Law Offices of Edward P. Shaughnessy today. Easton personal injury attorney Ed Shaughnessy has the specialized knowledge and resources needed to fight for the full compensation you deserve. He is committed to holding responsible parties accountable for their negligence. Call (610) 258-9955 or use the online contact form to schedule your free consultation.